
Treatment of Cavities
A cavity is a hole in the tooth that start small and grow over time if left untreated. Since many cavities do not cause discomfort at first, it can be difficult to recognize when the problem exists. Regular visits to the dentist can help in the early detection of cavities.
What is the treatment for Cavities?
Cavities are always treated with an appropriate diagnosis. Since permanently damaged enamel associated with dental caries may not be visible to the human eye, especially in the early stages, diagnosis requires expertise and modern tools. When our dental staff detects cavities, we develop a personalized treatment plan to remove the damaged enamel and preserve the tooth. Proper diagnosis and prompt treatment of dental caries are critical for a positive outcome. If left untreated, cavities can progress to a tooth abscess, which is an infection inside the tooth. Tooth abscess is much more painful and requires deeper treatment and you may lose the tooth.
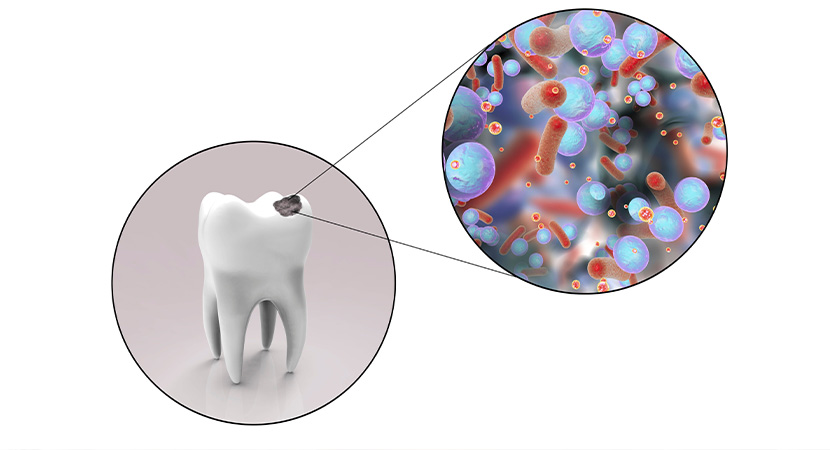
Cavities are permanently damaged parts of the hard surface of your teeth that turn into small hollows or holes. Cavities are caused by a variety of factors, including bacteria in your mouth, frequent snacking, drinking sugary beverages, and improper teeth cleaning. Cavities are among the most common health problems worldwide. They are most common among children, teenagers, and adults. However, cavities can affect anyone who has teeth, even newborns. Cavities become larger and damage the deeper layers of your teeth if not addressed. They can cause severe tooth pain, infection, and tooth loss. Your best defense against cavities is regular dental check-ups and proper brushing and flossing. Damage to the tooth surface or enamel is called caries. This happens when bacteria in your mouth produce acids that break down your tooth enamel. Cavities (dental caries) are holes in your teeth caused by caries. If left untreated, cavities can lead to discomfort, infection, and even tooth loss.

What causes Cavities?
Bacteria thrive in our mouths. Some bacteria are beneficial. However, some can be harmful, such as those that contribute to cavities. These bacteria interact with food to generate plaque, a soft, sticky coating. Plaque bacteria produce acids from the sugar and starch in your food and drinks. The acids begin to dissolve the minerals in your enamel. Over time, plaque can harden into tartar. Plaque and tartar, besides damaging the teeth, can irritate the gums and cause gum disease. Fluoride can be obtained through toothpaste, water, and other sources. This fluoride, along with your saliva, helps restore enamel by replenishing minerals. Throughout the day, your teeth go through this normal process of mineral loss and restoration. However, if you do not take care of your teeth and consume a lot of sweet or starchy foods, your enamel will continue to lose minerals. This causes tooth decay. When minerals have been lost, a white spot may form. This is a precursor to cavities. At this stage, you may be able to stop or reverse the degradation. If you take better care of your teeth and avoid sugary foods and drinks, your enamel can still be restored. However, as the deterioration process advances, more minerals are lost. The enamel deteriorates and erodes over time, leading to the formation of cavities. The dentist must use a filling to repair the damage.

Here's how tooth decay occurs:
1. Dental plaque is a sticky, transparent film that covers your teeth. It is caused by the consumption of high-carbohydrate foods and inadequate tooth cleaning. When sugars and starches are not removed from your teeth, bacteria feed on them and form plaque.
2. The acids in the plaque dissolve the minerals in the hard outer enamel of your teeth. This erosion creates microscopic gaps or holes in the enamel, which is the initial stage of cavity formation. When parts of the enamel wear away, the bacteria and acid can reach the dentin layer of your teeth.
3. Destruction continues. As decay progresses, the bacteria and acid continue to move through your teeth, nearing the inner structure of the tooth (pulp), which includes nerves and blood vessels. The bacteria cause swelling of the pulp and irritation.

Who is at risk of tooth decay?
Tooth decay can affect anyone with teeth; however, the following variables can increase the risk:
• Tooth location: Back teeth are most susceptible to decay (molars and premolars). These teeth have several crevices and edges, as well as multiple roots that can trap food particles. As a result, they are more difficult to clean than your smoother, more accessible front teeth.
• Certain foods and drinks: Milk, ice cream, honey, sugar, soda, dried fruits, cake, cookies, hard candies, and mint candies, dry grain foods, and chips are more likely to promote decay than products that are quickly washed away by saliva.
• Frequent snacking or drinking: Constant eating or consuming sweetened drinks provides oral bacteria with more fuel to generate acids that attack and wear down your teeth. Drinking soda or other acidic drinks throughout the day contributes to constantly washing your teeth with acid.
• Feeding infants before bedtime: When infants are given milk, formula, juice, or other sweetened drinks in their bottles before bedtime, these drinks linger on their teeth for hours while they sleep, feeding the decay-causing bacteria. This is sometimes called baby bottle tooth decay. When children drink from cups filled with these drinks, the same damage can occur.
• Inadequate brushing: Plaque builds up quickly after eating and drinking, and the initial stages of decay can occur if you don't clean your teeth immediately after eating and drinking.
• Insufficient fluoride intake: Fluoride, a naturally occurring mineral, helps prevent decay and can even reverse early stages of decay. Fluoride is added to many public water systems for its dental benefits. It is also a popular component of toothpaste and mouthwash. However, fluoride is rarely found in bottled water.
Tooth decay is common in many young children and teenagers in the United States. Older adults are also more vulnerable. Teeth can wear down, and gums can recede over time, making teeth more susceptible to root decay. Additionally, older adults are more likely to use medications that limit saliva flow, increasing the risk of decay.
If your mouth becomes dry, the lack of saliva causes dry mouth, which contributes to decay. Salivary substances also serve to neutralize the acid generated by bacteria. Some medications, medical conditions, head or neck radiation, and chemotherapy can increase the risk of decay by reducing saliva production.
Worn fillings can deteriorate, break, or develop rough edges over time. This makes it easier for plaque to form and makes its removal more difficult. They can loosen, allowing decay to develop underneath them.
Acids, also known as gastroesophageal reflux disease (GERD), cause stomach acid to enter your mouth (reflux), eroding enamel and causing significant tooth damage. This exposes more dentin to bacterial attack, leading to decay. Your dentist may advise you to consult a physician to determine if acid reflux is the source of enamel loss.
Eating disorders like anorexia and bulimia can cause severe erosion of the teeth and decay. Stomach acid washes over the teeth and begins to dissolve the enamel as a result of repeated vomiting (purging). Eating disorders can also disrupt saliva production.

What are the symptoms of tooth decay?
The signs and symptoms of tooth decay vary depending on the extent and location of the cavity. When decay is just beginning, you may not notice any symptoms. As the decay progresses, it can lead to signs and symptoms such as:
• Toothache, spontaneous pain, or pain that occurs for no apparent reason
• Sensitivity of the teeth
• Pain ranging from mild to severe when eating or drinking something sweet, spicy, or cold
• Visible pits or holes in your teeth
• Stains on the surface of the tooth that are brown, black, or white
• Pain when you bite down
• Infection, which can lead to the formation of an abscess (a pocket of pus). The abscess can cause discomfort, swelling of the face, and fever.
What are the complications of tooth decay?
Cavities are so common that you might think you can overlook them, right? And perhaps you think it doesn't matter if teenagers and babies develop cavities. However, tooth decay can have catastrophic and long-term consequences, even in youths who still don't have their permanent teeth.
Complications of cavities may include:
• Pain
• Tooth abscess
• Pus or swelling around the tooth
• Teeth that are damaged or broken
• Chewing problems
• Changes in tooth position following tooth loss
• When decay and cavities are severe, you may experience constant pain and bad breath
• Day-to-day living is hindered by pain.
• Weight loss or nutritional problems caused by painful or difficult eating or chewing
• Tooth loss can impact your appearance as well as your confidence and self-esteem.
In rare situations, a tooth abscess - a pocket full of pus caused by a bacterial infection - may develop, leading to more serious or even life-threatening conditions.

Can tooth decay be prevented?
Tooth decay can be prevented with good oral and dental care. Here are some guidelines to help you avoid cavities. Ask your dentist for the best advice for you.
• After eating or drinking, brush your teeth with toothpaste. Brush your teeth at least twice a day, preferably after each meal. Clean between your teeth with dental floss or use an interdental cleaner.
• Rinse your mouth with water. If your dentist believes you are at high risk of developing cavities, he or she may advise you to use mouthwash.
• Regularly visit your dentist. Get expert teeth cleanings and frequent oral exams to prevent or detect problems. Your dentist can advise you on the optimal schedule for you.
• Consider dental sealants. Sealants are plastic coatings placed on the chewing surfaces of the back teeth to protect them. They seal the grooves and crevices where food collects, protecting the tooth enamel from plaque and acid. Sealants are recommended by the Centers for Disease Control and Prevention (CDC) for all school-aged children. Sealants can last for several years before needing to be reapplied, but they should be checked regularly.
• When you consume fluids other than water, you help your oral bacteria produce acids that can damage tooth enamel. Your teeth are always under attack if you snack or drink throughout the day.
• Consume tooth-friendly foods. Some foods and drinks are more beneficial for your teeth than others. Avoid foods that linger in the grooves and crevices of your teeth for extended periods, or clean your teeth immediately after consuming them. Fresh fruits and vegetables, on the other hand, increase saliva production, while unsweetened coffee, tea, and sugarless gum help wash away food particles.
• Ask about antimicrobial medications. If you have a medical condition that makes you more susceptible to cavities, your dentist may recommend antibacterial mouth rinses or other treatments to help reduce harmful bacteria in your mouth.
• Tooth decay can be reduced by chewing gum containing xylitol.
How are tooth cavities diagnosed?
Diagnosing cavities is a simple process that our dentists can perform in one session; we often detect cavities during routine dental check-ups and in many cases identify signs of cavities before patients even notice symptoms. To diagnose cavities, we evaluate your symptoms, examine your teeth, and if there is suspicion of cavities, we take X-rays. We develop a treatment plan based on the facts gathered during our diagnosis. Your dentist will carefully inspect your teeth, looking for signs of cavities such as discoloration, enamel damage covering your teeth, or holes in your teeth. Our dentists will check for three types of cavities during your examination: smooth surface, pit and fissure, and deep cavities. Each affects a different part of the tooth. Smooth surface cavities form on the smooth surfaces of your teeth, while root cavities form on the surface of the tooth above the roots of your teeth. Cavities form on the chewing surfaces of your teeth. X-rays are used to see inside patients' teeth. Dense bone and tooth material appear white on X-rays, while soft tissues and cavities appear black. Healthy teeth appear white on X-rays. Since the nerve in the pulp is entirely made of soft tissue, it is black in color. Cavities appear as black spots on the tooth enamel. Our dentists use X-rays to diagnose cavities and assess the extent of deterioration.
What are the treatment options for cavities?
Cavities can be treated in various ways. The therapy you receive depends on the severity of the problem:
• Fluoride treatment: Fluoride treatment can help the enamel to self-heal if you have early-stage cavities.
• Fillings: If you have a normal cavity, your dentist will remove the decayed tooth tissues before filling the cavity with a filling. The dentist removes the decaying material from the tooth with a drill. Then your dentist will fill your tooth with composite resin.
• Root canal treatment: If the tooth is damaged or develops an infection towards the pulp (inside the tooth), you may need root canal treatment. Your dentist will clean the tooth and root and remove the decaying pulp. Then the tooth will be filled with a temporary filling. Then you will need to return for a permanent filling or crown (tooth covering).
• Extraction (tooth removal): In the most extreme situations, when the pulp damage cannot be repaired, your dentist may recommend tooth extraction. To replace the lost tooth, your dentist will recommend a bridge or implant. Otherwise, the teeth adjacent to the gap may shift and change your bite.
• Crown: If your tooth has significant deterioration, your dentist may place a custom crown on it to replace the natural crown. Before starting this process, your dentist will remove the decaying tooth material.
Conclusion
Cavities are holes in the teeth that occur when acids in the mouth constantly affect and break down the hard, outer coating of the tooth (enamel). Cavities can happen to anyone. Cavities can be avoided with proper brushing, flossing, and cleaning teeth with specialized waters and gels. Regular dental check-ups and proper oral hygiene are essential for preventing cavities. Newer dental treatments, such as dental sealants and fluoride rinses, have reduced the risk of cavities in children and adolescents. Adults with dental fillings from childhood may develop cavities around the edges of the previous fillings. Cavities in roots exposed by receding gums may also occur in adults.


