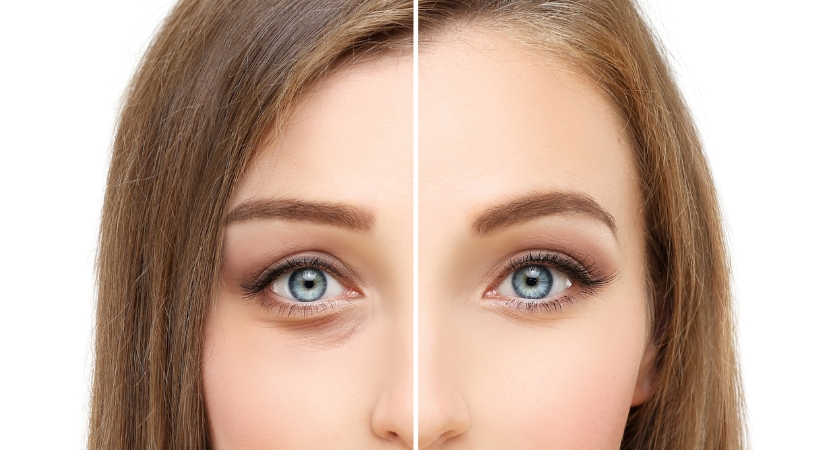
Are your lower eyelids baggy or puffy? Do you look tired or swollen all the time? Or do you have loose, wrinkled skin under your eyes? Lower eyelid bags can cause a lot of tension that can have a big impact on your life. Lower eyelid sagging can affect how you feel, both physically and psychologically, as well as how others see you.
Lower blepharoplasty, on the other hand, can remove lower eyelid bags and improve the texture of your eyelid skin, resulting in a smoother, more youthful appearance that improves your comfort and quality of life.
Lower blepharoplasty refers to a group of surgical procedures aimed at improving the appearance of the lower eyelids. Lower blepharoplasty used to be a reduction treatment in which skin and/or fat was removed to reduce lower eyelid creases, excess skin, and fatty bulges.
Although excision of fat and skin is still used in modern lower blepharoplasty, current developments adhere to a tissue-preserving philosophy that may include orbital and sub-orbicular fat transfer and fat transfer methods to restore the apparent volume loss associated with facial aging. Hyaluronic acid-based dermal fillers first emerged as a nonrelative method for lower eyelid and infraorbital volume in the early 2000s.
Non-surgical options for lower blepharoplasty or non-surgical adjuncts to incisional blepharoplasty have also been developed using laser energy and light therapies.

Structures of the eyelids
The eyelid is a movable tissue composed primarily of skin and muscle that covers and protects the eyeball from mechanical injury while contributing to the moist chamber, which is essential for proper conjunctival and corneal function. The conjunctiva, like the cornea, is a mucous membrane that borders the eyelid and covers the visible part of the eyeball (the transparent part of the eyeball that covers the iris and pupil). Each eyelid is supported by a fibrous plate known as the tarsus, as well as by muscles that move the eyelids and meibomian (or tarsal) glands that secrete lubricating secretions.
The eyelids are covered with skin, coated with mucous membrane, and fringed by hairs, the cilia. The eyelids move because of the activity of the orbicularis oculi, a circular muscle for closing the eyelids, and the upper eyelid elevator, a muscle lifting the eyelids. The facial (seventh cranial) nerve sends closing impulses, while the oculomotor (third cranial) nerve sends opening impulses. The sebaceous fluid (called sebum) of the meibomian glands keeps the eyelid margins moist. This secretion is incorporated into the tear film and helps to minimize tear loss on evaporation.
Why Lower Blepharoplasty?
The pre-operative medical and surgical history, as well as a physical evaluation of the patient's periorbital area (eyebrows to cheeks to nose), decide if the patient can safely undergo blepharoplasty treatment to resolve functional and cosmetic indications.
Blepharoplasty of the lower eyelid can successfully address the anatomic issues of excess eyelid skin, laxity of the eye muscles and orbital septum (palpebral ligament), excess orbital fat, malposition of the lower eyelid, and prominence of the nasojugal groove where the orbit (eye socket) meets the nasal slope.
The upper eyelid blepharoplasty procedure can correct peripheral vision loss caused by the upper eyelid skin overlying the eyelashes. The patient's peripheral and superior vision is impaired, making it difficult to perform everyday tasks such as driving a car and reading a book. Here are some common indications:
• Rhytidosis and dermatochalasis of the lower eyelid.
• Relative steatoblepharon.
• Pronounced nasojugal groove.
• Infraorbital/malar deflation.
• Malar mounds or festoons.
• Asymmetry of the lower eyelid.
• Retraction of the lower eyelid.
When is Lower Blepharoplasty contraindicated?
Patients seeking secondary benefits, such as improving their personal relationships, are not good candidates for cosmetic surgery. Patients who measure the effectiveness of surgery based on their happiness rather than recovery and reduction of age-related changes.
Any pathologic condition of the eyelids or orbital structures is an absolute contraindication. Any medical condition that may alter the patient's response to anesthesia, as well as unrealistic patient expectations, are considered relative contraindications
• Unattainable patient goals/unrealistic expectations.
• Concomitant severe or unstable medical conditions (e.g., uncontrolled HF, heart disease).
• Active thyroid ophthalmopathy (relative contraindication).
• Uncontrolled dry eye syndrome.

Preparation for surgery
You will meet with a plastic surgeon and an eye expert (ophthalmologist) or a plastic surgeon who specializes in eye procedures (oculoplastic surgeon) to discuss before scheduling your blepharoplasty:
• Your medical experience. Your surgeon will ask about previous surgeries, as well as past or current medical conditions, such as dry eyes, glaucoma, allergies, circulation problems, thyroid problems, and diabetes. Your doctor will also ask about prescriptions, vitamins, herbal supplements, alcohol, cigarettes, and drugs you take.
• Your expectations. An open discussion about your expectations and the reason for surgery can help set the stage for a successful outcome. Your surgeon will explain whether the surgery is likely to be successful for you.
Before your eyelid surgery, you will undergo:
• Physical examination - Your surgeon will perform a physical examination, which may include an assessment of your tear production and measurement of parts of your eyelids.
• Vision test - Your eye doctor will check your eyes and assess your vision, especially your peripheral vision.
• Eyelid photograph - Your eyes will be photographed from different angles. These photos help in planning the surgery, analyzing its immediate and long-term effects.
And you will be asked to:
• Stop using warfarin (Coumadin, Jantoven), aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, others), naproxen (Naprosyn), and any other medications or herbal supplements that are associated with increased bleeding.
• Ask your doctor how long you should wait before stopping these medications. Only take medicines prescribed by your surgeon.
• Stop smoking a few weeks before your procedure. Smoking may impair your ability to recover after surgery.
• If you are having outpatient surgery, arrange for someone to drive you there and back. Plan to have someone stay with you the first night after surgery.

Surgical options for Lower Blepharoplasty
Successful surgical rejuvenation of the lower eyelids resolves patient complaints that correspond to anatomical abnormalities discovered during the examination. The appropriate procedures and details may vary from surgeon to surgeon. A single technique or combination of procedures may achieve the desired result (e.g., manipulation of transconjunctival fat with anterior skin pinching).
Markings are often performed while the patient is seated. A surgical pen is used to draw the steatoblepharon and the borders of the indentations.
Local anaesthetic fluid containing lidocaine and/or bupivacaine with epinephrine is injected at the surgical site. A corneal shield may be used. It is necessary to use a sterile preparation.
Transconjunctival approach:
The transconjunctival approach is one of the most commonly used lower eyelid blepharoplasty procedures. It is an excellent alternative for people who have an abundance of fatty tissue on the lower eyelid, rather than extra skin on the lower eyelid. There are several approaches available, but one of the most common is discussed here.
A Desmarres retractor is used to provide access and an infratarsal incision is made using retractors on the conjunctiva and lower eyelid. Assessment of the orbital apples, helps in viewing the fat pads and finding the best location for the incision. Exposure is aided by traction sutures placed at the proximal conjunctival edge. If exposure is insufficient, lateral canthotomy and inferior cantholysis may be necessary. The orbital septum is not disrupted, allowing direct access to the three fat pads of the lower eyelid.
The orbital fat pads are removed or mobilized as pedicles to reposition them to sites of inferior recess, relative to the orbital rim. Monopolar or bipolar cauterization is used to maintain strict hemostasis. The inferior oblique muscle is visible and unaffected. After pocket generation and loosening of attachments, fat reaccumulation may occur in the suborbicular or subperiosteal plane. Percutaneous sutures or internal resorbable sutures are used to fix suborbicular ocular fat. Through a transconjunctival incision, the suborbicularis oculi fat (SOOF) can be elevated and fixed to the periosteum of the orbital rim using resorbable sutures. SOOF elevation, like orbital fat repositioning, assists in avoiding the lacrimal duct and infraorbital cavities.
Skin access (infraciliary):
An incision is made 1-2 mm below the lash line or within an existing infraciliary fold, extending to the lateral eyelid crease. By compressing the skin with a hemostat without creating traction on the lid margin, a "pinch" of the skin can be used to assess the degree of excess. Alternatively, a skin flap can be formed that extends as far as necessary to allow proper mobility while preserving the contour of the eyelid opening.
To avoid an anterior lamellar deficiency, only a small amount of skin is removed. To determine the amount of skin trimming that is permissible, the patient is asked to look up and open his mouth. The skin-muscle method begins with the flap deep to the orbicularis oculi and allows for improved advancement and trimming of skin and muscle as a separate entity or independently. The infraciliary incision allows access to the orbital fat pads and SOOF and is treated in the same manner as the transconjunctival approach.
Additional procedures:
Canthopexy or lateral canthoplasty is used to treat significant lower eyelid laxity prior to blepharoplasty.
Fat grafting procedures can be performed to increase the volume of the infraorbital grooves and the eyelid-cheek junction. Volumetric and projection defects can also be improved using alloplastic orbital rim and malar implants.
In eligible individuals, laser skin resurfacing (ablative or nonablative) or chemical peels improve lower eyelid skin quality and minimize rhytidesis and dyschromia.
Ligation, sclerotherapy, or laser treatment can help reduce or eliminate the appearance of unsightly lower eyelid veins.
Botox reduces dynamic wrinkles that appear in the periorbital area and lower eyelids.

What happens next?
After surgery, you will be monitored for problems in a recovery room. You can leave later that day to rest at home.
After surgery, you may experience:
• Blurred vision from the lubricating ointment applied to your eyes
• Watery eyes
• Light sensitivity
• Double vision
• Puffy, numb eyelids
• Swelling and bruising similar to black eyes
• Pain or discomfort
Your doctor will probably suggest that you take the following steps after surgery:
• At night after surgery, apply cold compresses to your eyes for 10 minutes per hour. The next day, apply cold compresses to your eyes four to five times during the day.
• Gently wipe your eyelids and apply prescribed eye drops or ointments.
• For one week, avoid exertion, weight lifting and swimming.
• For one week, avoid intense activities such as aerobics and jogging.
• Smoking should be avoided.
• Try not to rub your eyes.
• If you wear contact lenses, wait about two weeks after surgery before inserting them.
• Wear dark sunglasses to protect the skin on your eyelids from the sun and wind.
• Sleep with your head over your chest for a few days.
• To reduce swelling, apply cold compresses.
• Return to the doctor's office a few days later to remove any stitches.
• Avoid aspirin, ibuprofen (Advil, Motrin IB and others), naproxen sodium (Aleve and others), naproxen (Naprosyn) and other medications or herbal supplements that can cause bleeding for about a week. To relieve discomfort, take acetaminophen (Tylenol and others).
When should I call the doctor?
Seek medical attention immediately if you experience any of the following symptoms:
• Difficulty breathing
• Chest pain
• High heart rate
• New severe eye pain
• Bleeding
• Vision problems
Results of the procedure
Many people are pleased with the results of blepharoplasty, which include a more relaxed and youthful appearance as well as increased self-confidence. The effects of the surgery can last a lifetime in some people. Others may have recurrent droopy eyelids.
Bruising and swelling should disappear in 10 to 14 days, which is when you should feel safe going out in public again. Scars from surgical incisions may take several months to fade. Be careful not to expose your delicate eyelid skin too much to the sun.

Alternatives to Lower Blepharoplasty
Patients may prefer a nonsurgical eye lift to surgery for a variety of reasons. Anesthesia may not be an option for some, while others are concerned about the cost or downtime associated with surgery. Additionally, younger patients who exhibit only mild to moderate signs of aging may not believe their problems require invasive surgery at this time. Non-surgical alternatives to blepharoplasty can be effective in any of these situations.
Cosmetic injectables:
Injectable dermal fillers like JUVÉDERM® and wrinkle relaxers like BOTOX® can offer dramatic results with little to no downtime. The combination of fillers and neurotoxins can often help generate the most dramatic results by treating a variety of problems, such as hollowing under the eyes, dark circles under the eyes, and wrinkles or crow's feet around the eyes.
Radiofrequency (RF) microneedling:
Another wonderful non-surgical alternative for renewing the skin and generating a lifted, firmer, younger-looking eye area is radiofrequency microneedling. Specialized equipment will cause microscopic micro-injuries on the surface of the skin during RF microneedling, which uses a topical numbing medication to make the treatment more pleasant. This procedure destroys skin cells while stimulating the creation of new, healthy skin cells, resulting in a firmer, younger and more radiant complexion. Additionally, the radiofrequency energy stimulates cells deep beneath the skin to increase collagen and elastin formation, boosting benefits over the next several weeks and months.
Because the strength of RF microneedling can be adjusted, it is gentle enough to use on the delicate skin of the upper and lower eyelids, making it an excellent non-surgical alternative to blepharoplasty.
Platelet Rich Plasma (PRP)therapy:
Platelet-rich plasma treatment is another new option for rejuvenating the eyes without surgery. PRP is commonly used with microneedling to enhance its effects and generate even more stunning, longer-lasting results. During microneedling with PRP, a small amount of blood is drawn from the patient's arm. Specialized centrifuge equipment is used to separate the platelet-rich plasma from the other blood components. In addition, the microneedling device is passed over the skin, creating tiny punctures that encourage the growth of new, healthy skin cells on the surface. Finally, the PRP serum is massaged into the skin, enhancing the body's healing process as well as collagen and elastin production for firmer, younger-looking skin texture.
Laser Skin Repair:
With the availability of a variety of highly advanced ablative and non-ablative laser therapy systems, patients with virtually any skin type, tone, and color can address minor to severe issues and achieve desired results. Non-ablative treatments address more moderate issues and help regenerate skin and stimulate collagen synthesis, while ablative treatments address more severe symptoms such as severe sun damage and deep wrinkles.
Complications
• Retrobulbar hemorrhage is a rare but serious complication that must be treated urgently.
• Haemosis
• Pyogenic granuloma
• Insufficient or overcorrection of the steatoblefaron.
• Lagophthalmos
• Injury to the inferior oblique muscle/diplopia.
• Hypertrophic scar
• Suturing of cysts
Lower eyelid retraction is a risk in lower blepharoplasty and may be more prevalent when the septum is broken from the anterior approach rather than the transconjunctival approach. Scarring of the middle and/or posterior lid lamellae causes retraction, which is seen as a low-positioned eyelid that is connected to the orbital rim.
Excessive skin removal, unfavorable shrinkage after surgery, or poor healing after reconstruction of the eyelid skin surface can cause anterior lamellar deficiency.
Ectropion may occur after lower blepharoplasty, regardless of retraction or skin deficiency, if the lax lower eyelid does not heal or if postoperative traction forces are not resisted in the setting of poor canthal support.
Lower costs for Blepharoplasty
Lower blepharoplasty procedures are more expensive than upper blepharoplasty procedures because they are more difficult and often require general anesthesia, which increases costs. Basically, this technique is used to improve the appearance of the bags under a patient's eyes by reducing puffiness or tightening the skin just under the eye.
Conclusion
There is no doubt that a person's eyes affect their entire appearance. In fact, sagging eyelids and wrinkles around the eyes can make a person look tired, irritated, or older than they are. Because many of the first signs of facial aging appear on the eyelids and around the eyes, more and more people are opting for cosmetic eyelid surgery to bring back a more youthful appearance.
Lower blepharoplasty is a surgical method of treating eyelid abnormalities, deformities and distortions, as well as cosmetically altering the eye area of the face. Blepharoplasty treats functional and aesthetic problems of the periorbital area, which is the area between the eyebrows and upper cheek, by excising and removing skin and adipocyte fat and strengthening the appropriate muscle and tendon tissues. The surgery is most popular among women, who accounted for about 85 percent of blepharoplasty surgeries in the United States in 2014 and 88 percent in the United Kingdom.
The surgical goal of blepharoplasty is to restore proper function to the injured eyelid(s) as well as aesthetics to the surrounding facial area.


