
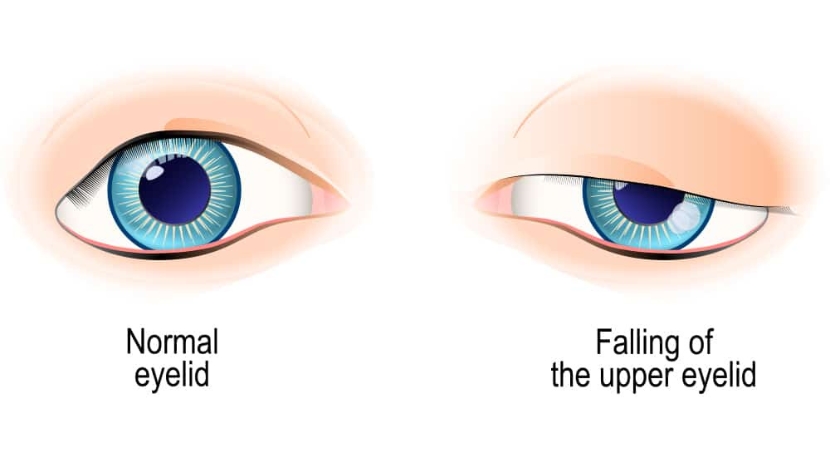
An ophthalmological condition known as blepharoptosis causes the upper eyelid to hang lower than it should. The upper eyelid usually covers the cornea by 1 to 2 millimeters. Blepharoptosis causes the eyelid to close even more, impairing vision. To see clearly, a person with this problem may need to manually lift their eyelid.
When the eye is in primary gaze, blepharoptosis refers to an abnormally low-lying upper edge of the eyelid. Typically, the top of the cornea is covered by 1-2 mm of the upper eyelid. Dermatochalasis, or an abundance of skin on the upper eyelid, is a distinguishing feature that can coexist with blepharoptosis. Since the surgical treatment of dermatochalasis and blepharoptosis is different, they must be identified.
Causes of Blepharoptosis
Both congenital and acquired blepharoptosis is possible.
Congenital Blepharoptosis
Isolated localized myogenic dysgenesis of the levator palpebrae superioris is usually the cause of congenital ptosis. A very small percentage of cases of congenital blepharoptosis may be caused by chromosomal or genetic abnormalities as well as by neurologic dysfunction.
Telecanthus, congenital ptosis, small palpebral fissures, and epicanthus inversus are hallmarks of blepharophimosis syndrome.
Congenital paralysis of the third cranial nerve.
Horner's congenital syndrome presents with mild ptosis, miosis, anhidrosis, and heterochromia.
Due to improper innervation of the ipsilateral elevator muscle from the motor nerve to the external pterygoid muscle, Marcus Gunn jaw wink syndrome develops. Patients experience lifting of the eyelids during chewing or after moving the jaw to the opposite side.
Acquired Blepharoptosis
The predominant variant of acquired blepharoptosis is aponeurotic. Stretching, dehiscence, or desensitization of the levator aponeurosis can cause aponeurotic blepharoptosis. When patients have aponeurotic blepharoptosis, it is also called involutional ptosis because the anatomic changes are age-related. Less common causes of acquired blepharoptosis include myogenic, neurogenic, traumatic, and mechanical factors.
Myasthenia gravis, chronic progressive external ophthalmoplegia, oculopharyngeal muscular dystrophy, and myotonic dystrophy are among the conditions that can cause myogenic blepharoptosis.
Horner's syndrome, a form of third nerve palsy, can cause neurogenic blepharoptosis.
After an eyelid laceration, there may be an incision of the upper eyelid elevators or a disruption of the neural circuit, both of which can lead to traumatic blepharoptosis.
An eyelid mass, such as a neurofibroma or hemangioma, or cicatrization resulting from infection or surgery can cause mechanical ptosis.

Pathophysiology of Blepharoptosis
Superior Levator Palpebrae and Mueller Muscle are the muscles that elevate the upper eyelids. The levator palpebrae superioris arises from the orbital apex, continues anteriorly, and courses as an aponeurosis inferiorly at the ligament of Whitnall. The anterior portion of the tarsal plate receives the aponeurosis. The fold of the upper eyelid is formed by attachments which it sends to the skin. The striated muscle, levator palpebrae superioris, is innervated by the superior subdivision of the oculomotor nerve. This muscle serves as the main elevator of the upper eyelid. The inferior aspect of the levator superioris is the origin of Mueller's muscle, a smooth muscle with sympathetic innervation. It extends for a length of about 12 mm, attaches superiorly to the tarsal border, and elevates the upper eyelid by about 2 mm. Damage to one or both upper eyelid elevator muscles causes blepharoptosis.
Symptoms of Blepharoptosis
History
Patients usually report that the affected eye is undersized, appears emaciated, has a limited range of vision, and have a headache. Any age can experience acquired blepharoptosis, but older people are more likely to experience it. From birth, congenital blepharoptosis manifests. Blepharoptosis has no predisposition to any one race or gender. Additional information regarding the onset of ptosis, aggravating or ameliorating factors, family history of ptosis, recent botulinum toxin injections, and history of trauma or ocular surgery is required. The history usually offers extremely strong information about the causes of blepharoptosis. To prevent potential complications after surgery, it is crucial to question anticoagulant use, family history of malignant hyperthermia, and cardiac disease.

Signs of Blepharoptosis
Documentation of refractive error and visual acuity is required. Eyebrow position and excess skin on the eyelids should be observed. A thorough external examination and palpation of the orbital rim and eyelids is important. The eyelid mass can add weight to the eyelid, which will cause blepharoptosis. The following measures should be taken before applying topical eye drops:
The space between the upper and lower eyelid in vertical alignment with the center of the pupil is known as a palpebral fissure.
The distance between the edge of the upper eyelid and the pupillary light reflex center with the eye in primary gaze is known as marginal reflex distance-1 (MRD-1).
The distance between the line of the lower eyelid and the pupillary light reflex centre with the eye in primary gaze is known as marginal reflex distance-2 (MRD-2).
When the frontalis muscle is kept passive at the brow, the elevation function is the distance the eyelids travel from the downward gaze position to the upward gaze position. A measurement of more than 10 mm is considered excellent, while a measurement of 0-5 mm is considered poor.
Presence of eyelid crease and its height
When a patient has unilateral blepharoptosis, the affected eyelid should be manually elevated, and the contralateral eyelid should be evaluated for any Herring phenomenon or masked blepharoptosis.
Examination of the patient is necessary to check for lagophthalmos, proptosis or enophthalmos and the presence of Bell's phenomenon. Because some patients with blepharoptosis may have limited ocular motility, such as in myasthenia gravis and chronic progressive external ophthalmoplegia, ocular motility should be evaluated. It is important to screen patients with congenital blepharoptosis for Marcus Gunn's jaw wink syndrome. Iris and pupil size discrepancies between the eyes should be examined for Horner's syndrome.
It is crucial to check the cornea, tear meniscus, and tear breakup time with fluorescein staining to see if dry eye is present. The Müllerian muscle can be stimulated using sympathomimetic eye drops. If a positive response is seen, a Mueller's muscle-conjunctival resection can be used to treat the ptosis.
Diagnosis of Blepharoptosis
For the majority of patients, a clinical examination is sufficient. The visual fields are usually checked to demonstrate the effects of blepharoptosis on peripheral vision. Detection of the source of blepharoptosis requires laboratory and imaging studies in a small number of cases.
Laboratory test
In patients suspected of having myasthenia gravis, a single fiber electromyography, a largefonium chloride test (Tensilon), and a serum acetylcholine receptor antibody assay may be ordered.
Electrocardiograms, electroretinograms, electromyograms, and mitochondrial analyses should be considered in patients with persistent progressive external ophthalmoplegia.
Diagnostic imaging
Patients with blepharoptosis and neurologic impairment should undergo imaging studies of the brain, orbits, or cerebrovascular system. Patients who have blepharoptosis and are thought to have inflammatory or infiltrative disease of the orbit should undergo a CT or MRI scan of the orbit. Imaging of the head and neck for acquired Horner's syndrome should be performed.
Treatment of Blepharoptosis
Surgery is the primary method of treatment for blepharoptosis. Observation is recommended only in mild cases of congenital ptosis where amblyopia, strabismus and abnormal head posture are absent. Surgery is performed as soon as possible if amblyopia, strabismus or significant abnormal head posture is likely. Blepharoptosis can be surgically corrected at any time to improve your field of vision or appearance.
Blepharoptosis should be reported to the appropriate physician for further treatment if it indicates systemic disease such as myasthenia gravis or Kearns-Sayre disease. Before attempting surgical intervention, it is recommended to gather external photographic documentation.
Medical treatment
Patients with myasthenia gravis may improve with medical care. In some patients, sympathomimetic topical eye drops such as apraclonidine and phenylephrine provide a brief, transient elevation of the upper eyelid. In July 2020, the FDA approved the use of topical oxymetazoline hydrochloride (0.1%) for blepharoptosis.
Surgery for Blepharoptosis
Depending on the severity of the condition, congenital ptosis can be surgically corrected at any age. Early intervention is necessary if amblyopia or severe aberrant head position is likely to develop. There are various surgical methods to correct blepharoptosis. The best procedure is chosen based on the goal of treatment, the underlying diagnosis, the surgeon's preference, and the level of levator function. Patients should understand that achieving symmetry is challenging. Patients with dry eyes, decreased corneal sensitivity, absent Bell's phenomenon, double elevator palsy, or progressive external ophthalmoplegia should be treated with extreme caution to prevent postoperative exposure keratopathy. The patient's strabismus should be treated first if blepharoptosis is also present.
Musculoconjunctival Mueller resection
Patients with mild to moderate aponeurosis blepharoptosis (these patients have very good levator function) may benefit from this approach. Even with strong elevator muscle function, this procedure does not work very well in patients with congenital blepharoptosis because the elevator palpebra muscle is abnormal. A positive response to topical sympathomimetic eye drops serves as a reliable predictor of the success of this type of surgery. Compared with other surgical methods, this one has the least likelihood of altering the shape of the eyelid.
For 1 mm blepharoptosis correction from the superior tarsal tip, the conjunctiva and Müller muscle are defined on the conjunctival side, and the defined conjunctiva and Müller muscle area are clamped. To remove the tissue above the clamp, a continuous suture is inserted under the clamp and externalized through the skin at either end of the defined area.
The Fasanella-Servat method of correcting ptosis is similar. However, the conjunctiva, Müller's muscle, and part of the upper tarsus must be removed. A stronger lift is obtained by incorporating part of the tarsal plate into the resection. The tarsus should not be removed excessively as this may compromise the structural integrity of the eyelid.
Advancement or resection of the levator
Depending on the degree of blepharoptosis, this procedure involves shortening the levator aponeurosis. Patients with good and acceptable levator function (>5 mm) may benefit from it.
An incision in the eyelid crease is used for the procedure. The preaponeurotic fat is retracted from the levator aponeurosis as the orbital septum is opened. The levator aponeurosis separates from the tarsus once the muscle is localized, and dissection can then proceed between the levator aponeurosis and the Müller muscle. The levator aponeurosis is then advanced and/or removed and temporarily attached to the tarsus with one to three threads and partial-thickness bites. The degree of blepharoptosis determines the degree of advancement and/or removal. At this point, if the patient is conscious, the height and shape of the eyelid are checked. The tarsal lamellar bites are then permanently tightened after reaching the appropriate height and shape. To restore the fold, the skin is closed by inserting a portion of the aponeurosis of the levator.
Frontal suspension
Patients with inadequate (4 mm) or absent levator function undergo this treatment. Multiple autogenous and allogenous materials can be used as slings. Frontalis muscle flaps and fascia lata, preserved fascia lata (from a tissue bank), autologous temporal fascia, silicone, Alloderm, and Gore-Tex sutures have been used. It has been found that the most successful surgical outcome is achieved with autogenous fascia lata. The levator connects the eyelid and eyebrow and when the eyebrow is lifted, the eye opens. After surgery, patients may take several months before they can close their eyelids while they sleep. Considerable lubrication is needed during this time.
The greatest cosmetic result in patients with unilateral severe blepharoptosis is achieved by bilateral frontal sling. However, convincing the patient and family to undergo surgery on the healthy contralateral elevator muscle is often challenging.
The surgical method of restoring blepharoptosis of the mandible in patients with Marcus Gunn syndrome is controversial. Depending on the degree of ptosis and levator function, restoration of blepharoptosis alone (with levator advancement or frontonasal sling) may be adequate if the jaw wink is minor. Extirpation of the elevator muscle and implantation of a frontalis sling may be necessary if the jaw wink is severe.
Tracking Blepharoptosis
Blepharoptosis surgery is usually performed as outpatient surgery. To reduce swelling and bruising, apply cold compresses to the eyes for 20 minutes every 1-2 hours for 2-3 days. Patients are given topical antibiotic ointment (with or without steroid) to apply twice daily for 5-7 days to the incision site and eye. Excessive lubrication is necessary in patients in whom surgical lagophthalmos is expected. After surgery, patients are often reviewed one to two weeks later. Patients are evaluated for over- and undercorrection, infection, granuloma formation, exposure keratopathy, and other ocular conditions. Patients with amblyopia should continue treatment.
Complications of Blepharoptosis
Amblyopia due to deficient or untreated astigmatism may result from congenital ptosis. Frontal headaches and limited visual field are effects of acquired blepharoptosis. The significant psychosocial impact of blepharoptosis can lead to poor academic and occupational performance.
Bleeding, infection, edema, under- or overcorrection of ptosis, eyelid asymmetry, granuloma formation, corneal foreign body sensation, and exposure keratopathy can complicate surgical correction n of blepharoptosis. Most of these problems are relatively manageable if identified early and treated appropriately.
Prognosis for Blepharoptosis
Available medical and surgical treatments for blepharoptosis usually yield positive results. Over time, recurrence is not uncommon. This result may require multiple surgeries, especially in cases of congenital ptosis.
Conclusion
Patients seeking oculoplastic surgery often have upper eyelid blepharoptosis. Although there are many different types of ptosis, simple congenital ptosis in young patients and senile ptosis in adults are the two most common clinical presentations. It is crucial to differentiate between these and other, less common types of ptosis, such as those that are neurogenic, myogenic, and posttraumatic, by examining the patient. These latter conditions may require special therapeutic approaches. Surgery is usually an effective way to treat ptosis.


