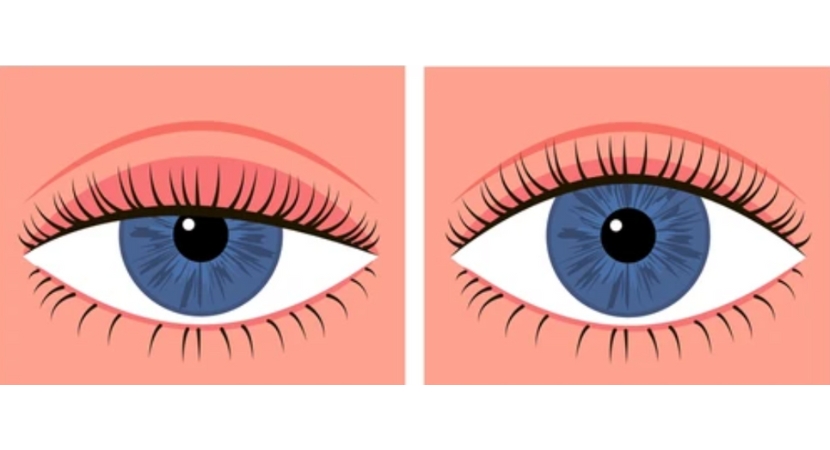
The term "ptosis" comes from the Greek word meaning "falling" and refers to the drooping of a part of the body. Blepharoptosis is the drooping of the upper eyelids with eyes in a predominantly upward position. The shape of the eyes, as well as the position of the eyelids and the shape and position of the eyebrows, establish a person's identity. As a result, droopy eyelids can lead to functional or aesthetic deficits.
Ptosis can occur at any age and can be caused by various reasons. It is important to note that when a patient complains of drooping, it is only a symptom, not a diagnosis. A comprehensive evaluation is needed to determine the cause.
Definition of Ptosis
Ptosis refers to the drooping of a particular part of the body, especially the eyelid. Eyelid ptosis can occur and affect one or both eyelids. This involves the drooping of the upper eyelid, partially covering the pupil. This leads to a sleepy, tired appearance and reduced vision. In most cases, a corrective procedure is necessary to address the problem and improve vision.
In this case, ptosis correction is primarily recommended. Its aim is to correct the droopy eyelids to give you a lively and more youthful appearance. Professional ophthalmologists specialized in eyelid surgery typically perform the correction procedure. Besides ample experience, this type of surgery requires appropriate attention to detail in planning and executing the operation.

Anatomy and Physiology of Upper and Lower Eyelids
The palpebral fissure is an oval opening between the upper and lower eyelids. The curvature of the upper eyelid is greatest just nasal to the midpoint of the pupil, which is a critical landmark for marking before surgery to achieve the best aesthetic effects. The upper eyelid covers 1 to 2 mm of the upper limbus, while the lower eyelid is situated at the lower limbus.
Structures forming the eyelid:
• Skin and subcutaneous tissue
• Orbicularis oculi
• Orbital septum
• Preaponeurotic fat pad
• Tarsal plate
• Levator aponeurosis and Müller's muscle
• Conjunctiva
Skin
The skin of the eyelids is the thinnest layer of skin on the body. The levator aponeurosis attaches to the skin and forms the eyelid crease.
Orbicularis Oculi
This is a circular muscle with three sections: preseptal, pretarsal, and orbital orbicularis. Contraction is responsible for both gradual and forced closure of the eyelids.
Orbital Septum
It is composed of several layers of thin fibrous connective tissue. The septum attaches to the periosteum above the upper orbital rim. It connects to the fibers of the levator aponeurosis below the upper tarsal border. The septum is opened during ptosis surgery to provide access to the lifting muscle. To minimize postoperative eyelid retraction, the septal attachments to the lifting muscle must be carefully dissected.
Preaponeurotic Fat Pad
The fat pad is located behind the septum and in front of the levator. Intraoperatively, this fat pad can be identified by applying pressure on the globe, causing it to prolapse forward. It assists in identifying the lifting muscle, which lies just behind it.
Tarsal Plate
The tarsal plate is a sturdy connective tissue structure that forms the structural skeleton of the eyelid. The upper eyelid has a vertical height of 10 to 12 mm, while the lower eyelid has a vertical height of 4 to 5 mm. The Meibomian glands are located in the tarsal plates, and their openings are situated behind the gray line.
Levator Palpebrae Superioris Muscle (LPS)
The primary elevator of the eyelid is the LPS. It arises from the periosteum above the lesser wing of the sphenoid near the orbital apex. It moves forward beneath the orbital roof. It switches direction from horizontal to vertical near the upper orbital rim and produces the tendon sheath known as the lifting aponeurosis. The Whitnall ligament, seen as a dense white band of connective tissue and functioning as a pulley, is located at this transition. It is positioned 10 to 12 mm above the tarsal plate.
There are various insertions of the levator aponeurosis. It inserts into the skin of the upper eyelid anteriorly, forming the eyelid crease. It inserts from below onto the anterior surface of the upper one-third of the tarsus. It is attached to the upper conjunctival fornix posteriorly. It generates the medial and lateral horns, which subsequently insert into the posterior lacrimal crest and tubercle of Whitnall, as well as the canthal tendons.
Müller's Muscle
This is smooth muscle that is sympathetically innervated. It arises from the undersurface of the levator aponeurosis at the level of the Whitnall ligament and inserts into the upper tarsal border. It contributes to a 2 mm elevation of the eyelids.
Conjunctiva
This is the deepest layer of the eyelid, composed of non-keratinizing squamous epithelium. It extends over the entire anterior surface of the eye orbit. It includes goblet cells, the secretions of which are crucial for maintaining the eyes moist.

Understanding Common Types of Ptosis
Ptosis of the eyelids is usually divided into two main categories, including:
Congenital Ptosis
The condition of congenital ptosis is present at birth and may remain undiagnosed until childhood. At this stage, it tends to become more apparent. This occurs when the lifting muscle responsible for elevating the eyelid does not mature properly. Congenital ptosis of the eyelids impairs the upper part of the visual field. As a result, children with the disorder often tilt their heads back to see properly.
If Congenital Ptosis is left untreated, it can lead to other vision problems such as amblyopia or lazy eye.
Acquired Ptosis
While some people may be born with ptosis, others acquire the condition later in life. It may occur when the connections or muscles that naturally lift the eyelid weaken after illness or injury. Sometimes, drooping may occur due to damage to the nerves controlling the eyelid muscles.
Acquired Ptosis of the eyelids exists in various forms, including:
Mechanical Ptosis: This develops when the eyelid is forced downward due to excessive tissue mass or skin.
Aponeurotic Ptosis: Aponeurotic ptosis is the most common type of ptosis in adults and typically occurs in the fifth or sixth decade of life. Sometimes called involutional ptosis, it can develop in young individuals as a result of trauma, recent eyelid swelling, eye surgery, or long-term use of contact lenses. The most common cause of aponeurotic ptosis is dehiscence or disinsertion of the levator aponeurosis. True dehiscence may sometimes be absent in involutional cases, and ptosis arises due to stretching or thinning of the aponeurosis. Fatty infiltration of the levator muscle is uncommon.
Patients with this type of ptosis have excellent lifting function with a high eyelid crease; the affected eyelid appears lower on downward gaze and has a thin upper eyelid with excess skin.
Neurogenic Ptosis: This type of condition is caused by a problem related to the nerve pathways that regulate the movement of the eyelid muscles. Third nerve palsy, Horner's syndrome, and myasthenia gravis are examples of these conditions.
Ptosis and limitation of eye movement in adduction, elevation, and depression of the eyeball are symptoms of oculomotor nerve lesions. Pupillary involvement may be present or absent. The Bell phenomenon is often ineffective. Third nerve palsy involving the pupil is a neurological condition caused by an aneurysm of the posterior communicating artery compressing the nerve.
Third nerve palsy sparing the pupil is most commonly caused by an ischemic vascular source and usually resolves spontaneously within 3 months. Other causes include inflammation, injury, or tumors along the nerve pathway. Lesions in the superior orbital fissure, orbital apex, or cavernous sinus occur in association with other cranial nerve palsies.
Traumatic Ptosis: This occurs after trauma or injury to the eyelid, altering the lifting muscle.
Myasthenia Gravis
Myasthenia gravis is an autoimmune disease characterized by antibodies against acetylcholine receptors located at the neuromuscular junctions of voluntary muscles. This leads to decreased cholinergic activity, resulting in muscle weakness and fatigue. Myasthenia can be generalized or specific to the eye (ocular myasthenia).
Variable ptosis with diplopia is the most typical presenting feature. Unilateral or bilateral symptoms are possible. Patients with myasthenia initially have normal levator function. Prolonged upward gaze exacerbates ptosis in these patients due to muscle fatigue.
The ice test, serum antibody analysis against acetylcholine receptors, single-fiber electromyography, and repetitive nerve stimulation test are additional procedures that can help confirm the diagnosis.

Evaluation of Patients with Ptosis
A detailed history and clinical examination help determine the cause of ptosis and plan appropriate therapy.
History
The age of onset of ptosis, progression, duration, and any exacerbating or alleviating variables should be included in the history. All accompanying symptoms, such as diplopia, daily fluctuations, discomfort, eyelid swelling, dysphagia, or muscle weakness, assist in the preliminary diagnosis.
Trauma, eye or eyelid surgery, contact lens use, and botulinum toxin injection should be carefully evaluated as risk factors. To rule out genetic disorders, a family history of ptosis should be sought. When the patient's history is ambiguous, examination of historical photographs may help determine the onset period.
Documentation of any systemic illness, mental health issues, or medication history is necessary. Patients using blood thinners, such as aspirin, should be instructed to stop their medications one week before surgery.
Clinical Examination
The clinical examination begins the moment the patient enters the doctor's office. Facial asymmetry, frontalis hyperactivity, elevated chin, or tilted head posture are observed.
Eye Examination
• Refraction and Visual Acuity
• A covert examination to search for hypotropia and rule out any components of pseudoptosis.
• Disruption of extraocular motility, as well as any unusual eyelid movements.
• Examination of the pupil for Horner's syndrome or third cranial nerve palsy.
• Inspect the eyes for significant papillary conjunctivitis or symblepharon.
• Corneal sensation and dryness in the eyes should be assessed as they may lead to postoperative keratopathy.
• Examine the fundus for signs of retinal pigment degeneration.
Indications for Ptosis Correction
The majority of patients seeking ptosis treatment do so because of blurred vision and loss of peripheral vision caused by the drooping eyelid. Another typical complaint is heavy eyelids. A significant portion seeks surgery for aesthetic reasons, as droopy eyelids create a tired appearance.
Contraindications
• Severe dryness in the eyes.
• Patients with myogenic ptosis, such as persistent progressive external ophthalmoplegia - if ptosis correction is planned for these patients, conservative surgery to preserve visual axis should be considered.
• Bell's phenomenon.
• Ptosis associated with oculomotor nerve paralysis.
• Myasthenia gravis: These patients should first be treated with anticholinesterase drugs.

What does Ptosis Correction involve?
Ptosis correction aims to lift the upper eyelid, which causes blurred vision and an asymmetric appearance. This typically helps improve the visual field as well as cosmetic characteristics. There are several different surgical methods that doctors use to lift the eyelid. The specific type of technique to be applied depends on the underlying cause of the ptosis.
For proper determination of the height of the upper eyelid, maximum calmness and cooperation are necessary. As such, the procedure is usually performed under local anesthetics applied through the eye. After applying eye anesthetic drops, local anesthesia is injected directly into the eyelid. This helps numb the area where the procedure is to be performed.
When it comes to performing the procedure, the doctor may choose either surgical approaches for lifting the muscle or for brow suspension.
Levator Muscle Advancement
This is the most common type of ptosis surgery. It involves making an incision in the natural skin crease of the upper eyelid. Through the incision, the doctor will identify the levator muscle, which lifts the eyelid. It is then reattached or advanced forward to strengthen it, with dissolvable stitches used for closure. The skin incision in the eyelid crease is sutured with the help of dissolvable stitches, which usually fall off on their own within a few weeks. Sometimes it may be necessary to return to the hospital to have them removed.
Brow Suspension Surgery
This technique is used when the patient has a levator muscle that is unusually thin or weak. While some children are born with the condition, others may acquire it as they grow. To attach the upper eyelid to the forehead, a plastic material is used, along with non-dissolvable thread. Alternatively, the doctor may harvest tissue from the upper thigh to use as a sling. The eyelid is then lifted using the muscles of the forehead. The procedure requires two incisions on the upper eyelid, two incisions just above the eyebrow, and a small incision on the forehead.
Preparing for Ptosis Correction
Before the corrective surgery, you and the doctor will meet to further discuss the procedure. Typically, ptosis correction surgery is a personal decision. Therefore, it is practical to do it only if it is safe and after consultation with a doctor.
You will be instructed to stop taking blood thinners like aspirin before the procedure. Also, make sure you have informed the doctor if you are using any herbal medication. In most cases, they may ask you to stop taking them at least 14 days before the surgery.
Smoking interferes with the recovery process. Therefore, you should try to quit at least six to eight weeks before surgery, if necessary at all. If you have high blood pressure, make sure it is under control, as it will increase the risk of severe bleeding and bruising.
Don't forget to bring a list of all current medications, as well as details of any allergies you have. There is no doubt that you will be able to return home on your own after treatment. But it's best to have someone accompany you after you're discharged.
Postoperative care for Ptosis Correction
Expected mild discomfort includes:
• Swelling usually subsides after 1 week.
• In rare cases, swelling may take several weeks to resolve.
• Avoid exertion and rest with your head elevated at 30 degrees to speed up swelling reduction.
• Bruising typically disappears after 2 weeks.
• Tearing.
• Lagophthalmos.
• Incomplete eyelid closure – usually transient.
• Eye drops with lubricant or eye gel may be needed to prevent corneal drying.
• An eye shield may be necessary during sleep.
Postoperative medications:
• Apply antibiotic ointment regularly 3-5 times a day.
• Antibiotic eye drops 3 times a day.
• Oral antibiotics.
• Analgesics (pain relief) and anti-swelling medications.
• Sutures removal after one week.
• Light activity can be resumed after 3-4 weeks.
• Avoid wearing contact lenses for at least 4 weeks after surgery.
What to Expect After Ptosis Correction
After ptosis surgery, it is normal to experience pain and discomfort. Most often, the doctor will prescribe some pain relievers such as ibuprofen. Bleeding may occur in the area of the surgery. Therefore, you should apply pressure with a clean pad for at least 10 to 15 minutes to alleviate the bleeding.
Always ensure that the incision is clean. You can use warm boiled water or sterile saline solution and clean cotton gauze to clean the area. It is also important to apply ointment or eye drops at least four to six times a day for one or two weeks. This ensures that the eyes remain lubricated throughout.
Swelling and bruising are common after the procedure. You can use an ice pack or apply cold compresses to alleviate the condition. The speed of swelling and bruising recovery varies from one patient to another. However, it is likely to subside within two to three weeks. Sometimes it may extend to the upper part of the cheeks, leading to swelling of the lower eyelid bags. However, this will fade over time.
Most people usually resume their normal daily activities within two to three days after the procedure. However, you should refrain from strenuous activities for at least two weeks after surgery. This improves the healing process and allows the wounds to heal well. Also, avoid direct sunlight as it may interfere with the healing process of the scars. You may consider wearing sunglasses on sunny days while recovering.
The eyelid bruising and the white line will gradually fade over time. Fortunately, most eyelid scars are hidden by the natural folds of the eyelids.
Risks and Complications of Ptosis Correction
• All types of surgical procedures carry various risks of complications. Ptosis correction, on the other hand, is also associated with a number of risks that may arise during or after the surgery. These include:
• Swelling and bruising around the surgical area.
• Blurred vision is often a result of the eye drops and ointments used.
• Watery eyes due to irritation and pain.
• Chemosis (swelling of the conjunctiva, the transparent covering of the eye).
• Dry eyes. After the surgery, you may experience reduced blinking and limited eye closure for several days or weeks. Doctors recommend using artificial tears to alleviate the condition.
• Asymmetry of the eyelids. Sometimes it is difficult to achieve equal height for each eyelid after surgery. Therefore, a small difference may be noticed.
• Inability to properly close the eyelids for several days after surgery. It may be difficult to fully close the eyes if the eyelids are lifted too high.
• Eyelid contour defects, where the eyelid crease looks unusual due to swelling. Sometimes another surgery may be required.
• Scarring. Although incision wounds often heal well, unusual scars may appear on the eyelid and deeper tissues.
• Loss of sensation, especially when nerves are damaged or cut. This can cause numbness in the area of the incision.
• Asymmetry, where the area of the eyelids and face are uneven.
• Hematoma (bleeding around the eyeball).
• Infection.
• Additional surgery.
Conclusion
Ptosis of the eyelids is a medical condition that can affect both children and adults. It is characterized by drooping of the upper eyelids, partially obstructing the visual field. Doctors often recommend ptosis correction to address such impairments. In addition to improving overall vision, the procedure also enhances cosmetic appearance.
Ptosis correction helps restore the visual field and improves aesthetic appearance. It alleviates the feeling of heaviness in the eye. Most patients feel and look younger, improving their quality of life.


